Low Blood Pressure- Understanding Hypotension
Blood pressure, the force exerted by circulating blood on the walls of blood vessels, is a vital parameter that keeps our cardiovascular system functioning optimally. While high blood pressure (hypertension) has long been in the spotlight due to its association with various health risks, the converse – low blood pressure (hypotension) – often remains in the shadows. Yet, understanding the symptoms of low blood pressure is crucial for maintaining overall well-being and preventing potential complications.
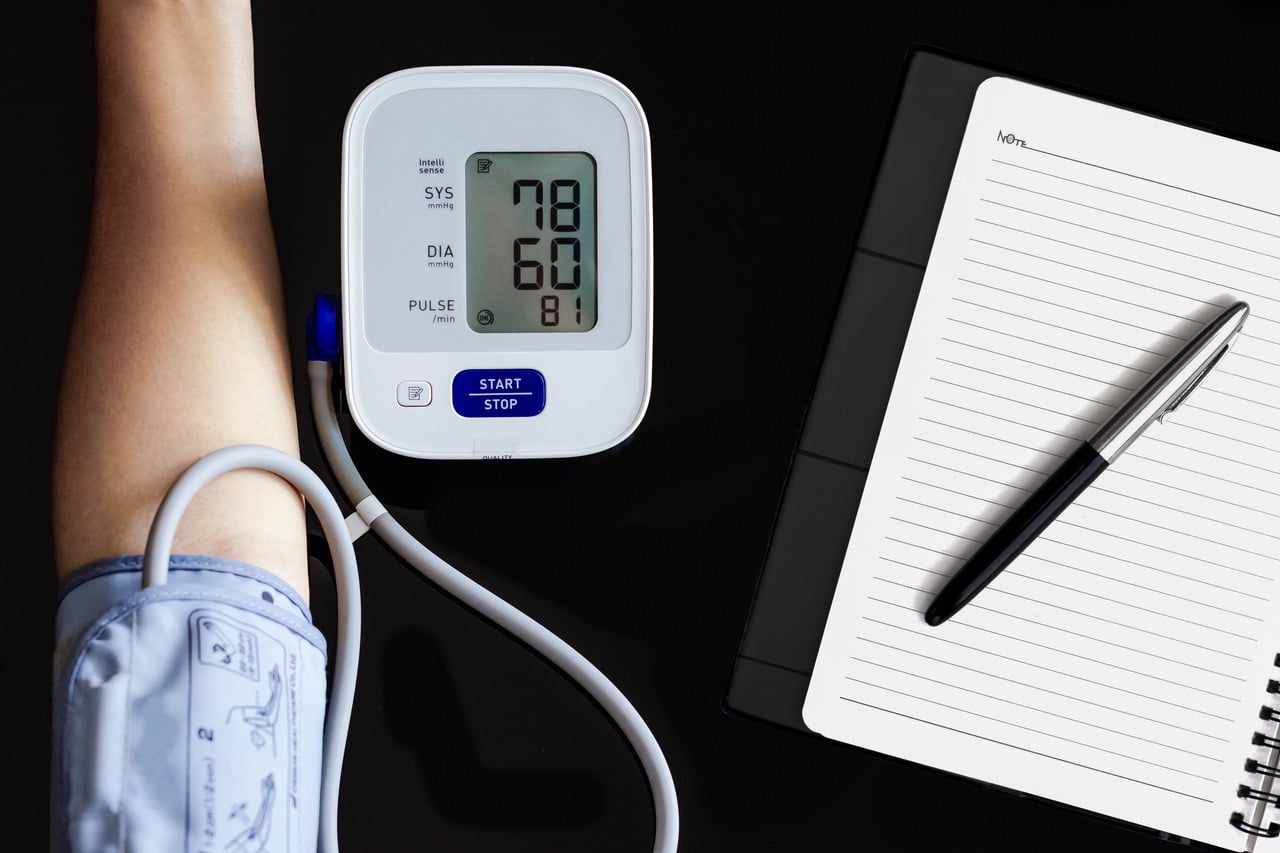
In this article, we embark on a journey to uncover the subtle cues that our bodies provide when blood pressure takes a dip below the norm. Low blood pressure, defined as a reading lower than 90/60 mm Hg, can manifest through an array of symptoms that might be mistaken for other ailments or even overlooked entirely. By delving into these signs, we shed light on the importance of recognising low blood pressure and taking proactive steps towards addressing its underlying causes.
Blood Pressure Ranges
Understanding the various ranges of blood pressure is essential for recognizing deviations from the norm and identifying potential health concerns. Blood pressure readings are typically expressed as two values: systolic pressure (the higher value) and diastolic pressure (the lower value). These measurements reflect the force of blood against arterial walls during different phases of the heartbeat.
Normal Blood Pressure Range
A normal blood pressure reading falls within the range of approximately 90/60 mm Hg to 120/80 mm Hg. This range is considered optimal for maintaining healthy cardiovascular function and minimizing the risk of associated health issues.
Low Blood Pressure (Hypotension)
Hypotension occurs when blood pressure consistently measures below 90/60 mm Hg. While low blood pressure is not always indicative of a serious health problem, persistent hypotension can lead to inadequate blood flow to vital organs, potentially causing symptoms and complications.
Orthostatic Hypotension
A temporary drop in blood pressure upon standing, resulting in dizziness or lightheadedness. This can occur due to sudden changes in position, prolonged bed rest, or dehydration.
High Blood Pressure (Hypertension)
Hypertension is characterized by blood pressure readings that consistently exceed 130/80 mm Hg. Prolonged high blood pressure can strain the heart and blood vessels, increasing the risk of heart disease, stroke, and other health issues.
- Stage 1 Hypertension: Systolic pressure ranging from 130 to 139 mm Hg, or diastolic pressure ranging from 80 to 89 mm Hg.
- Stage 2 Hypertension: Systolic pressure of 140 mm Hg or higher, or diastolic pressure of 90 mm Hg or higher.
Why Blood Pressure Ranges Matter
Maintaining blood pressure within the normal range is vital for overall health and well-being. Deviations from these ranges can indicate potential health concerns and warrant further evaluation. Low blood pressure may lead to symptoms like dizziness, fainting, and fatigue, while high blood pressure can strain the heart and damage blood vessels, increasing the risk of serious cardiovascular events.
Factors Contributing to Low Blood Pressure
Low blood pressure, or hypotension, can be influenced by a variety of factors that impact the body’s ability to regulate blood flow and maintain appropriate blood pressure levels. Understanding these factors can provide insights into the potential causes of low blood pressure and guide individuals in taking proactive measures to address them.
Dehydration
Insufficient fluid intake can lead to a decrease in blood volume, resulting in lower blood pressure. Dehydration can be caused by factors such as inadequate water consumption, excessive sweating, vomiting, or diarrhoea.
Medications
Certain medications, particularly those used to treat high blood pressure (antihypertensives), heart conditions, and some psychiatric disorders, can unintentionally lead to a drop in blood pressure. It’s important to be aware of the potential side effects of medications and consult a healthcare provider if you experience symptoms of hypotension.
Heart Conditions
Weakness in the heart muscle, irregular heart rhythms (arrhythmias), and heart valve disorders can compromise the heart’s ability to pump blood effectively. Conditions like bradycardia (slow heart rate) can contribute to low blood pressure.
Endocrine Disorders
Hormones play a crucial role in regulating blood pressure. Disorders of the adrenal glands (such as Addison’s disease) and thyroid dysfunction can disrupt hormonal balance, leading to hypotension.
Nutritional Deficiencies
Inadequate intake of essential nutrients, particularly vitamin B12 and folic acid, can impact blood pressure regulation. These nutrients are essential for the proper functioning of the nervous system, including the autonomic nervous system responsible for regulating blood pressure.
Prolonged Bed Rest
Extended periods of immobility, such as bed rest following surgery or illness, can cause blood to pool in the legs. When you stand up, this pooled blood may not be effectively pumped back to the heart, resulting in a sudden drop in blood pressure known as orthostatic hypotension.
Neurological Conditions
Certain neurological disorders, such as Parkinson’s disease, can disrupt the autonomic nervous system’s control over blood pressure regulation, leading to hypotension.
Pregnancy
Low blood pressure is common during pregnancy due to hormonal changes, increased blood volume, and changes in blood vessel tone. Most cases are mild and temporary.
Summary
Low blood pressure, or hypotension, can result from factors affecting blood flow regulation and maintenance of proper pressure levels. Dehydration, caused by inadequate fluid intake or conditions like vomiting and diarrhoea, can reduce blood volume and pressure. Medications, including those for hypertension and heart issues, can inadvertently lower blood pressure. Heart conditions like weak muscles or irregular rhythms, endocrine disorders such as adrenal and thyroid problems, and nutritional deficiencies (e.g., vitamin B12, folic acid) can disrupt pressure regulation. Prolonged bed rest may lead to orthostatic hypotension, pooling blood in the legs upon standing. Neurological disorders like Parkinson’s can affect blood pressure control. In pregnancy, hormonal changes and increased blood volume can induce temporary low blood pressure.
Common Symptoms of Low Blood Pressure
Low blood pressure, or hypotension, is often referred to as a “silent” condition due to its inconspicuous nature. However, the body provides a range of signals and symptoms that can serve as crucial indicators of hypotension. Recognising these signs is essential for timely intervention and the prevention of potential complications. In this section, we explore the diverse array of symptoms that may accompany low blood pressure.
A. Dizziness and Lightheadedness
Sudden changes in position, such as standing up quickly, can cause a momentary drop in blood pressure, leading to feelings of dizziness and lightheadedness. Individuals with Postural Orthostatic Tachycardia Syndrome (POTS) may experience an abnormal increase in heart rate upon standing, coupled with dizziness.
B. Fainting or Near-Fainting (Syncope)
A common type of fainting triggered by factors like emotional stress, pain, or standing for extended periods. It occurs when blood pressure drops and the heart rate slows down.
C. Fatigue and Weakness
Low blood pressure can impede the delivery of oxygen to the body’s cells, resulting in decreased energy levels. Insufficient blood flow to muscles and tissues can lead to feelings of fatigue and weakness.
D. Blurred Vision
Low blood pressure can affect blood flow to the eyes, leading to blurred or dimmed vision.
E. Nausea and Vomiting
Low blood pressure can trigger nausea and vomiting due to reduced blood flow to the digestive system.
F. Cold, Clammy Skin
In an effort to redirect blood flow to vital organs, the body may constrict blood vessels in the extremities, resulting in cold and clammy skin.
G. Rapid, Shallow Breathing
Hypotension can disrupt the balance of oxygen and carbon dioxide exchange in the lungs, leading to shallow breathing.
H. Difficulty Concentrating
Reduced blood flow to the brain can result in difficulty focusing, poor concentration, and cognitive fog.
I. Increased Heart Rate (Tachycardia)
The heart may respond to low blood pressure by increasing its rate in an attempt to maintain sufficient blood flow.
Summary
Low blood pressure, known as hypotension, often goes unnoticed due to its “silent” nature, but the body presents a spectrum of symptoms as vital indicators. Recognizing these signs is pivotal for timely intervention and averting complications. These symptoms encompass dizziness upon sudden movement, fainting triggered by factors like stress, fatigue stemming from reduced oxygen delivery, blurred vision, nausea, cold skin due to redirected blood flow, rapid shallow breathing, difficulty concentrating, and an elevated heart rate as the heart compensates for low pressure. Understanding and heeding these symptoms are imperative for effective management and prevention.
Lifestyle Management and Prevention
While low blood pressure may have a variety of causes, adopting a proactive approach to lifestyle management can play a significant role in preventing and alleviating its symptoms. Making informed choices in daily routines, diet, and physical activity can help regulate blood pressure and enhance overall cardiovascular well-being. In this section, we explore strategies for managing and preventing low blood pressure through lifestyle adjustments.
A. Hydration and Fluid Intake
Adequate fluid intake is crucial to maintaining healthy blood volume. Aim to drink enough water throughout the day, especially in warm weather or during physical activity. Furthermore, include foods rich in electrolytes, such as potassium and sodium, to support proper fluid balance in the body.
B. Balanced Diet
If advised by a healthcare professional, adding a moderate amount of salt to your diet can help raise blood pressure. Consume a balanced diet with ample fruits, vegetables, whole grains, lean proteins, and healthy fats to support overall health.
C. Gradual Posture Changes
When transitioning from sitting or lying to standing, do so gradually and avoid sudden movements to allow your body time to adjust and minimize the risk of orthostatic hypotension.
D. Physical Activity
Engage in moderate exercise routines that promote cardiovascular fitness and help maintain healthy blood pressure levels. If you have a medical condition or are on medications, consult your doctor before starting a new exercise regimen.
E. Nutritional Supplementation
Ensure you’re getting adequate vitamin B12 and folic acid through your diet or supplements, as deficiencies can contribute to low blood pressure.
F. Avoid Triggers
Limit alcohol intake and monitor your caffeine consumption, as both can influence blood pressure. Avoid prolonged exposure to hot environments, which can lead to blood vessel dilation and lower blood pressure.
G. Manage Stress
Engage in relaxation techniques such as deep breathing, meditation, and yoga to help manage stress and regulate blood pressure.
H. Regular Medical Check-ups
Schedule regular appointments with a healthcare professional to monitor your blood pressure, discuss symptoms and adjust treatment plans if needed.
Summary
Maintaining optimal blood pressure involves a holistic approach. Adequate fluid intake, including electrolyte-rich foods, supports healthy blood volume. A balanced diet, potentially with moderate salt intake, complements exercise to promote cardiovascular fitness and overall health. Gradual posture changes mitigate orthostatic hypotension risks, while stress management techniques like meditation aid blood pressure regulation. Ensuring sufficient intake of vitamin B12 and folic acid, monitoring alcohol and caffeine, and avoiding prolonged heat exposure contribute to balanced blood pressure. Regular medical check-ups with healthcare professionals enable monitoring, symptom discussion, and treatment plan adjustments. This comprehensive strategy empowers individuals to proactively manage and safeguard their blood pressure levels.
When to Seek Medical Attention
While mild instances of low blood pressure may not always warrant immediate medical attention, certain situations and symptoms indicate the need for prompt evaluation by a healthcare professional. Recognizing when to seek medical help is crucial in preventing potential complications and addressing underlying health concerns. In this section, we outline scenarios that require medical attention for individuals experiencing low blood pressure.
A. Acute Symptoms
- Severe Dizziness or Fainting: If you experience frequent or severe episodes of dizziness, lightheadedness, or fainting, especially after changing positions, seek medical help to rule out underlying issues.
- Chest Pain: Persistent or sudden chest pain, discomfort, or pressure may signal heart-related problems and should be evaluated immediately.
B. Symptoms Impacting Daily Life
- Unexplained Fatigue: If you consistently feel overly tired, weak, or fatigued despite adequate rest and nutrition, consult a healthcare professional.
- Difficulty Breathing: Shortness of breath, rapid breathing, or shallow breathing should be addressed, especially if they interfere with daily activities.
C. Symptoms in Specific Populations
- Elderly Individuals: Older adults are more vulnerable to the effects of low blood pressure. If they experience falls, confusion, or increased frailty, medical attention is essential.
- Pregnant Women: Pregnant individuals with persistent low blood pressure or symptoms like dizziness should consult their healthcare provider.
D. Symptoms Accompanied by Medical Conditions
- Underlying Medical Conditions: If you have a pre-existing medical condition such as heart disease, diabetes, or thyroid disorders, consult your doctor if you notice changes in your blood pressure or experience related symptoms.
- Medication Side Effects: If you suspect that medications are contributing to low blood pressure, consult your healthcare provider to discuss potential adjustments.
E. Changes in Medication
If your healthcare provider changes your medication regimen or dosage, closely monitor your blood pressure and report any noticeable changes or adverse effects.
F. Unusual or Severe Symptoms
Neurological Symptoms like confusion, difficulty speaking, weakness on one side of the body, or sudden vision changes should be treated as medical emergencies.
G. Persistence of Symptoms
If you experience ongoing symptoms such as persistent dizziness, fatigue, or fainting, it’s essential to consult a healthcare professional for a comprehensive evaluation.
Summary
Recognising when to seek medical attention amidst low blood pressure instances is pivotal for averting complications and addressing underlying health issues. While mild cases might not necessitate immediate medical care, specific symptoms and scenarios warrant prompt evaluation by healthcare professionals. Acute episodes of severe dizziness, fainting, and chest pain, especially after position changes, necessitate investigation. Symptoms impacting daily life like unexplained fatigue and breathing difficulties warrant attention. Vulnerable populations like the elderly, pregnant individuals with persistent symptoms, and those with pre-existing conditions should seek medical help. Medication side effects, changes, and unusual or severe symptoms require immediate attention, as do persistent symptoms like dizziness, fatigue, or fainting. By heeding these indicators, individuals can prioritize their health and ensure timely management of low blood pressure concerns.
HealthifyMe Suggestion
Low bp or hypotension is characterised by various symptoms such as dizziness or lightheadedness, fainting, blurred vision, fatigue, nausea, cold, clammy skin and or rapid, shallow breathing. If you feel any of such symptoms to start with you should replenish your body with electrolytes. You can use, sugary drinks, lemon water, candy, etc. If the symptoms still persist. Seek immediate medical attention.
Conclusion
In the intricate landscape of cardiovascular health, low blood pressure emerges as a silent yet significant player. While its subtle symptoms often go unnoticed, understanding the mechanisms, triggers, and implications of low blood pressure is paramount for maintaining overall well-being. From the momentary dizziness that accompanies a swift change in posture to the persistent fatigue that raises questions about our vitality, the body’s signals are valuable guides on this journey.
Through this exploration, we’ve unravelled the factors contributing to low blood pressure, from dehydration and medication interactions to heart conditions and nutritional imbalances. Equipped with this knowledge, we can forge a proactive path towards better health. Lifestyle adjustments, such as staying hydrated, embracing a balanced diet, engaging in appropriate physical activity, and managing stress, emerge as crucial allies in maintaining optimal blood pressure levels.
Yet, the importance of knowing when to seek medical attention cannot be understated. As we’ve outlined, there are times when low blood pressure requires more than just lifestyle adjustments. Acute symptoms, persistent challenges, and scenarios unique to certain populations demand the expertise of healthcare professionals for accurate diagnosis and tailored guidance.
Ultimately, our journey into low blood pressure serves as a reminder that health is a multifaceted voyage. By heeding our bodies’ signals, embracing a comprehensive approach to well-being, and seeking the guidance of medical experts when needed, we navigate the path towards a life marked by vitality, awareness, and the full embrace of our cardiovascular health.
Disclaimer: The purpose of this article is just to disperse knowledge and raise awareness. It does not intend to replace medical advice from professionals. For further information please contact our certified nutritionists Here
Frequently Asked Questions (FAQs)
What is low blood pressure (hypotension)?
Low blood pressure, or hypotension, refers to abnormally low pressure of blood against the walls of arteries. It can result in inadequate blood flow to vital organs and tissues.
What are the common symptoms of low blood pressure?
Common symptoms include dizziness, lightheadedness, fainting, fatigue, nausea, blurred vision, and rapid heart rate.
What is considered a low blood pressure reading?
Blood pressure below 90/60 mm Hg is generally considered low.
Can low blood pressure be a cause for concern?
Yes, persistent low blood pressure can lead to reduced blood flow to organs and may cause symptoms or complications.
Are there different types of hypotension?
Yes, different types include orthostatic hypotension (related to position changes) and neurally mediated hypotension.
What are the potential causes of low blood pressure?
Causes include dehydration, heart conditions, endocrine disorders, medication side effects, and more.
How is low blood pressure diagnosed?
Diagnosis involves blood pressure measurement, reviewing symptoms, and considering medical history.
Can low blood pressure be linked to other medical conditions?
Yes, it can be associated with heart problems, neurological disorders, and more.
Are there lifestyle changes that can help manage low blood pressure?
Yes, staying hydrated, a balanced diet, regular exercise, and stress management can help.
Can dehydration contribute to low blood pressure?
Yes, dehydration reduces blood volume, leading to low blood pressure.
